Frequently Injured Workers, when attending workers’ compensation evaluations and treatment are asked to fill out a lot of questions and forms. One of these forms that they may have to fill out is the Wong-Baker FACES® Pain Rating Scale.
These Scales can impact an Injured Worker’s industrial claim.
This article will discuss the Wong-Baker FACES® Pain Rating Scale, how It is used in a Workers’ Compensation claim, and how it can impact an Injured Worker’s claim.
What is the Wong-Baker FACES® Pain Rating Scale?
The Wong-Baker Pain Rating Scale is a tool which is used to allow for patients to provide a self- assessment of their pain. It was created by Donna Wong and Connie Baker in 1983 to help children communicate about their pain. .
Part of the goal is to improve the assessment by using the scale for the purposes of assisting in pain management. The Wong-Baker Faces Foundation indicate that the Scale is self-assessment tool [that] must be understood by the patient, so [that[ they are able to choose the face that best illustrates the physical pain they are experiencing. The Foundation note that the Scale is “not a tool to be used by a third person, parents, healthcare professionals, or caregivers, to assess the patient’s pain. There are other tools for those purposes”.
What Does the Scale Look Like? How It is Scored?
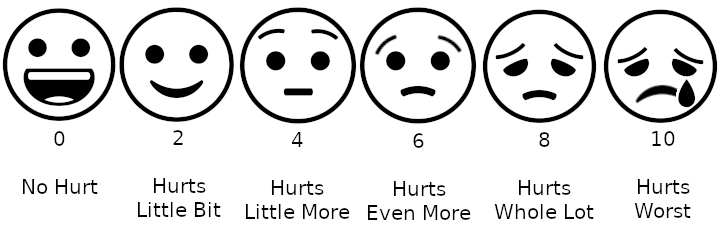
The picture above is a version of the scale. This picture was taken off of the Wikipedia article. The Scale is copyrighted. The Scale is proprietary. Therefore, if you are interested in the material you should contact the Foundation.
The instructions for its usage is to “explain to the person that each face represent a person who has no pain(hurt), or some, or a lot of pain.” “Face 0 doesn’t hurt at all. Face 2 hurts just a little bit. Face 4 hurts a little bit more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have his worst pain.”
The person is asked to choose the face that best depicts the pain they are experiencing. Supra.
Besides the Scale, the Patient may be asked to “to mark their areas of pain on a drawing of a human figure then rate each area using the faces scale.”.
What Was This Scale Designed for? What is Your Opinion Concerning It?
Originally, it was designed for children to help them communicate their pain.
In California, there are a number of Injured Workers who do not speak English. There are some Injured Workers who are illiterate. Some are illiterate even in their language of origin. This type of Pain Scale can assist these individuals express themselves with respect to their pain. It is noted by the Foundation that for children there was “considerable difficulty using any scale with unfamiliar words or scales based on numbering or ranking concepts. The use of the Numeric Rating Scale [were] growing in popularity at this time, but young children had trouble using the numbers.” Thus, this type of scale is of some value with certain Injured Workers.
With respect to other workers, the Scale is more problematic. In the world of workers’ compensation, there is a focus on activities of daily living and how an injury impacts them. This particular scale, while it may be effective with respect to ascertaining pain information for other reasons, does not provide information used for disability assessment in the workers’ compensation system.
With respect to Adults, pain is viewed must differently than with children. Adults react to pain as an irritation, a distraction, frustration, and may generate anger and upset. Adults do not necessarily cry because of their pain. Most adults, however, can understand how the scale signifies a range from no pain to extreme pain. In sum, its inquiry is superficial. Again, this is not an indictment of the Scale, it is simply the problem that occurs when it is employed for something it was not intended for.
How Can The Wong-Baker Scale Be Used For In Workers’ Compensation?
In my opinion, the Scale may have some credibility value. Also, it may document the trajectory of an Injured Worker’s condition. If this Scale is used on multiple occasions, one can look to see how consistent the reporting it. Also, it can possibly bring light to possible exaggeration. Scores at level 10 may give rise to suspicion of exaggeration.
Any Advice Concerning the Scale?
It is very important for Injured Workers to try to be accurate with respect to the score. While providing a “10” may be a “cry for help,” I would suggest that the Injured Worker actually “cry for help” and tell the evaluator or treater that they are experiencing some level of frustration with respect to their treatment and their relief from the pain. This will prevent an allegation of exaggeration.
What If I Need Advice?
If you would like a free consultation concerning any workers’ compensation case, please contact the Law Offices of Edward J. Singer, a Professional Law Corporation. They have been helping people in Central and Southern California deal with their worker’s compensation cases for 28 years. Contact us today for more information.